Osteoarthritis (OA)
What is Arthritis/OA?
The term ‘Arthritis’ refers to a group of conditions involving inflammation of joints in the human body. The most common form of arthritis is osteoarthritis (OA). OA occurs when cartilage (the smooth coating between bones) wears down – leading to undesired frictional contact and a repeating inflammatory process.
It may affect any joint in the body but most commonly affects the hands, knees, hips, lower back, and neck. OA is now understood to be a distinct disease process with different stages, as opposed to simply being age-related wear and tear of the joint surface.
What should I expect?
OA is a progressive disease that worsens over time. While there is no complete cure, there are many interventions that may be used to minimize pain and keep yourself mobile/active.
What are some symptoms of OA?
- Pain during/after activity or at the end of the day
- Swelling at involved joints
- Stiffness, especially in the morning or after periods of rest
- Reduced movement
- Clicking or cracking with movement
- Weakness
- Instability (feelings of ‘buckling’ or ‘giving way’)
Who does it affect?
OA commonly starts in middle age, often in the 40’s/50’s and seems to affect women more than men. It may, however, occur earlier as a result of prior injuries or repetitive use of the joint over time. Whilst it is very common, some people never develop the disease.
Some other factors that may contribute to developing OA include
- Older Age
- Obesity
- Weak muscles at/around the affected area
- Genes
- Hips – lifting heavy loads regularly as a part of work (such as in labour work)
- Knees – regular squatting, climbing, kneeling
How do I know if I have it?
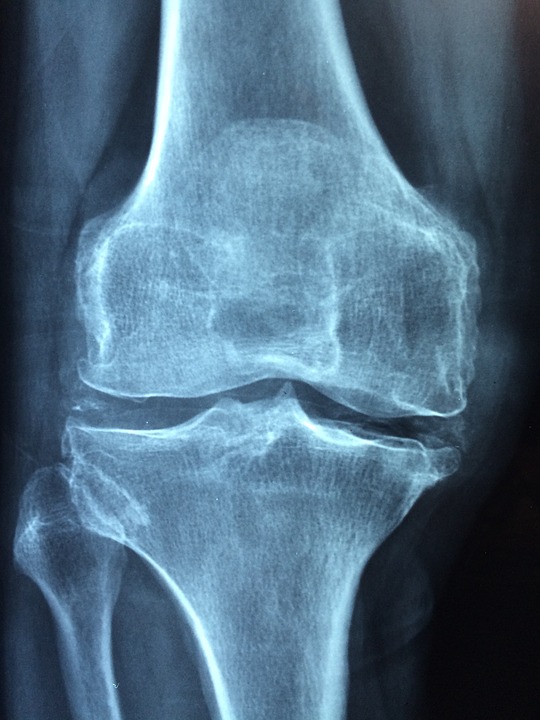
Your treating practitioner will make a diagnosis based on your reported symptoms and physical assessment. An X-Ray may be ordered to show the extent of arthritic changes in the joint.
What are some things that can help?
Exercise! – The current health guidelines suggest completing 150 minutes of moderate to vigorous exercise each week. Guidance should always be sought from a health professional when beginning an exercise plan to ensure that it is appropriate and safe.
- Strengthening – such as half squats, calf raises, or step ups
- Stretching/range of motion – such as yoga poses or daily movement exercises to get joints moving
- Weight bearing exercise – Has been proven to be safe and beneficial for arthritic joints.
- Cardio – such as brisk walking, stationary biking, or swimming.
- Hydrotherapy – Aquatic therapy in warm water is a great way to promote movement with less pain.
- Balance training – such as slow marching on the spot or standing with a narrow stance/on one leg.
Diet – Maintaining a healthy weight and sustaining a controlled diet can reduce the amount of pressure being placed through arthritic joints.
Medications – including NSAIDS, pain relievers, or corticosteroids – these can help to reduce inflammation and keep the pain controlled. Pain medication may be taken before/after exercise to allow more activity.
Icing – can be used as a tool to ease swelling and minimize pain when a joint has become aggravated.
Braces/Shoe inserts/Assistive devices – The use of such items should be considered (after consultation with a healthcare practitioner) to help you achieve/tend to daily activities more comfortably.
Injection – The treating physician may prescribe a platelet rich plasma or cortisone injection to reduce pain/promote healing. Research shows, however, that these have variable success rates.
Surgery – If the disease has progressed heavily your doctor may recommend you see a surgeon to replace the damaged joint. This surgery aims to restore movement to the joint and decrease your pain
References:
Arthritis foundation US – https://www.arthritis.org/diseases/osteoarthritis
https://arthritisaustralia.com.au/types-of-arthritis/osteoarthritis/
https://www.mayoclinic.org/diseases-conditions/osteoarthritis/diagnosis-treatment/drc-20351930